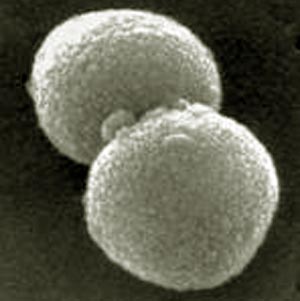
Streptococcus Pyogenes
What is Streptococcus Pyogenes?Streptococcus pyogenes is one of the gram-positive cocci in chains overlap. The cell walls of streptococcal cells has some interesting features. The high content of peptidoglycan (murein layer) of carbohydrate (C polysaccharide) gives the cells a very strong structure. The C-polysaccharide antigen is effective. It is in some species, especially beta-hemolytic streptococci, species-specific and is then called a group antigen. By the American microbiologist Rebecca Lancefield established classification of streptococci and enterococci D in the serological groups A, B, C, etc. based on these antigenic. Streptococci of serological group A belong to the species Streptococcus pyogenes. As a further antigen in Streptococcus pyogenes has the M-protein. This feature allows the subdivision into serovars. The typing relies today mostly on the sequencing of the genes of the M proteins (emm genes). Currently more than 150 different emm-types are known. The M protein has an antiphagocytic effect. |
Streptococcus Pyogenes pathogenesis
Reservoir of Streptococcus pyogenes is the human. In particular, the throat is colonized, preferably in the winter months. As virulence is the M protein, which enables the propagation of the streptococci in the host only. The cell wall peptidoglycan and especially the complex of C polysaccharide exerts a tissue toxicity, which also emanates from dead cells of streptococci. They also provide a number of group A streptococcal exotoxins. The haemolysins streptolysin O and S destroy the membranes of red blood cells and other cells. Streptolysin O acts as an antigen that can be detected by measuring antibodies against this toxin (antistreptolysin titer). The pyrogenic streptococcal exotoxin (PSE) A, B, C are responsible for fever, rash, and scarlet, and enanthema in sepsis and toxic shock syndrome. They act as superantigens, causing a release of large amounts of cytokines. The enzymes streptokinase, DNAse and hyaluronidase favor the spread of infection in the tissue. Streptococcus pyogenes infection is one of the most common infectious diseases. They usually occur in children with a peak in the age group of 4 - to 7-year-old on. The number of acute streptococcal pharyngitis in Germany is estimated at 1 to 1.5 million per year. Only a portion of infections are clinically apparent, ie the reservoir is mainly the larger droplets by direct contact or transmitted pathogens. The incubation period ranges from one to three days. Among the diseases must be between acute infection and subsequent invasive disease (see below) can be distinguished. The pathogens invade the broken skin or mucous membranes and cause local infections that may develop into sepsis. In the vast majority of infections of the upper respiratory tract is affected. Starting from the streptococcal pharyngitis, which manifests itself mostly as a high fever, exudative tonsillitis, peritonsillar abscess can arise, sinusitis or other complications. Scarlet fever is a special form of streptococcal pharyngitis, observed with the addition of a speckled rash of angina (and enanthema) is. A second group of diseases are infections of the skin (pyoderma, impetigo, erysipelas) dar. a very serious disease is necrotizing fasciitis, with or without the myositis. The special feature of this infection is the sudden onset of symptoms, rapid progression in normally healthy people, and the toxic shock syndrome. The pathogens produce exotoxins A, B and rarely C. An important long-term consequence is the acute rheumatic fever, an inflammatory disorder that occurs after a streptococcal infection of the respiratory tract. It can manifest itself to the heart, joints, nervous system, skin and subcutaneous tissue (hypodermis). The reason for this is a cross-reactivity between M protein and cellular components of muscle cells (myosin and tropomyosin). The incidence is estimated at two cases per 100,000 population. Further complications are acute glomerulonephritis, and a type II immune disease. |
Streptococcus Pyogenes diagnosis

The diagnosis is made by the culture test (determination of the serogroup) on blood agar plates. Are based on a currently available rapid antigen detection tests according to the Robert Koch Institute is not sensitive enough. Antibody detection assays are useful only in cases of suspected streptococcal sequelae.
Streptococcus Pyogenes therapy
Resistance to penicillin (various trademarks) has not been observed. First-line therapy is therefore the 10-day dose of penicillin (orally or parenterally). See www.ndrugs.com for medications. In penicillin allergy a macrolide antibiotic is considered. However, 8-15% of isolates are resistant to macrolides. The spectrum of activity of telithromycin (Ketek) also captures the majority of macrolide-resistant strains. Fluoroquinolones and cotrimoxazole (EUSAPRIM, COTRIM HEXAL FORTE, etc.) do not work reliably. In severe systemic infections (sepsis, toxic shock syndrome, necrotizing fasciitis), the administration of parenteral penicillin in combination with clindamycin (Sobelin, CLINDAHEXAL etc.) is recommended. Patients with rheumatic fever should receive a relapse prevention with benzathine penicillin (TARDOCILLIN etc.). They should be given at least five years, for life after a relapse.